How can we face chronic pain?

- 3836
- 823
- Glen Vandervort Sr.
"If you here and now it is intolerable and makes you miserable, you have three options: withdraw from the situation, change or accept it totally". Eckhart Tolle
At present, thanks to the advancement of research in neurosciences, it has been observed that there is greater decrease in pain when it comes to it in a comprehensive manner, Taking into account biopsychosocial aspects, both to determine the causes and for their treatment, since they can directly influence the reduction of pain perception.
The traditional orthodox treatment for chronic pain, had focused more on biomedical aspects, Walsh and Radcliffe (2002), showed that Patients treated in a multidisciplinary way, to a greater extent their perception of pain, while those who valued their pain as an organic condition presented greater degree of disability.
Content
Toggle- Prevalence of pain
- Acute pain and chronic pain
- Coping strategies against chronic pain
- Smart actions to face chronic pain
- Breastfeeding and chronic pain
- Deadaptive coping strategies
- Conclusion
- Links
Prevalence of pain
The presence of chronic pain in the world is significant, they estimate that between 25 and 29% of the population suffers pain, It is estimated that in Europe 20% of the population manifests chronic pain (2017). It is usually more common among women and individuals of limited economic resources, to developing countries, where most people do not even have basic health or education services, can be a great challenge, both for health professionals and for which what suffer, so I know They can benefit affecting psychological variables involved in chronic pain.
Acute pain and chronic pain
If you suffer chronic pain, you could remember: how many times before your condition reached such degrees, you ignored the needs of your body, which sometimes whispered you and sometimes I shouted that you stopped and stopped for a moment to listen to it and attend it? The hustle. If you do not suffer, you may be time to start listening more attention to your body.
Acute pain warns us that something is wrong, instead chronic pain affects different tissues, we have specific receptors to collect painful information, it travels through the spinal cord and reaches the brain to process it, therefore, it depends largely on psychological factors: The way in which experience and coping strategies chosen by the person can cause pain are perceived, maintain or decrease.
The pain serves as an alert system, warns the individual of harmful agents or threats for their body, whether real, potential or perceived simply. Thus, prepare the person in a physiological and cognitive way, contributing to survival, People who cannot feel pain are unable to live beyond adolescence.

Chronic pain is a condition that as such must be treated by specialists in it and in a multidisciplinary way, regularly implies emotional discomfort for which it manifests it, so a comprehensive treatment contemplates the help of a psychologist trained in the management of chronic diseases ; the CIE-11 (International Disease Classification) states that chronic pain is one that remains for more than three months, either intermittently or persistently.
 Gemotherapy and its benefits in the body and mind
Gemotherapy and its benefits in the body and mind Coping strategies against chronic pain
Behavior to pain According to the adjustment made by the person with their condition and their environment, It can be adaptive or maladaptive. The first, involve dynamic and optimal coping strategies before the "invader" that has been installed for a long time inside the body trying to tyrannize it, often consuming the well -being of the person.
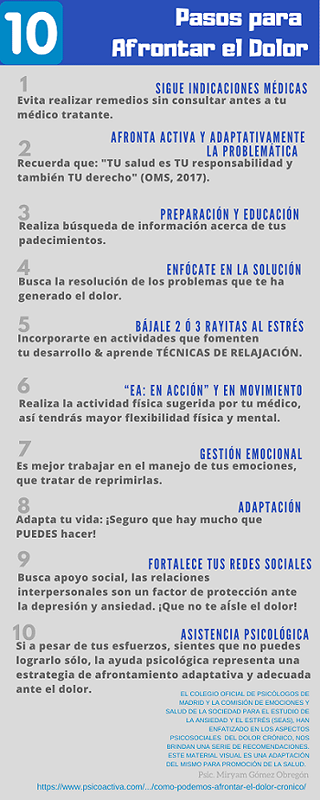
Smart actions to face chronic pain
An adequate coping strategy is to attend with pain specialists, follow medical suggestions and seek psychological accompaniment, since the emotional suffering of the person can make more pain experience, If there is comorbidity with psychopathologies, your condition is more complicated.
Finding mutual help groups, who share chronic pain and other conditions they present, can represent an adequate coping strategy, the life stories of many can motivate the person, when pain punishes the body, tears are many and seem to be that The torment has no end. However, due to comorbidity with many psychopathologies, they suggest psychological assistance to influence cognitive factors that could help perceive less pain. The most frequent psychological problems among patients with chronic pain are depression and anxiety.
Another positive aspect of the help groups is that together they seek novel information about their condition, it is recommended that be accompanied by health professionals, who can contribute to well -being, people suffering from pain can be easy prey of those who look precisely With the pain and suffering of others, before practicing the remedy that served a pain of pain, it is necessary to ask your head doctor before, if that remedy for your evil is adequate. Ignorance can be very pernicious, Education on these issues can empower us to face pain with the best weapons, such as good warriors.
Active coping strategies against pain go aimed at solving problems and information search. Other coping strategies before adaptive pain are:
- Smart Movement: Perform the recommended physical activity with the frequency and duration indicated.
- Follow food suggestions and sleep hygiene.
- Perform a heavy metal detoxification.
- Strengthen support networks with loved ones and people who can be seen.
- Ensure recreational activities according to their tastes and faculties.
- Enjoy sexuality.
- Laugh.
- Stroke and hug loved beings, let themselves caress and hug for them; If you have pets, caressing them can also be therapeutic.
- Join a circle of reading, of a theme that interests you.
- Practice breathing, relaxation, full attention and meditation techniques.
- Music therapy.
- Sublimar emotions through the arts.
- Listen to your body and meet your basic needs.
- Use the imaginative resource for the reinterpretation of pain sensations.
- Decrease stress levels so that pain mechanisms work optimally.
- Massages approved by the treating doctor in conjunction with an experienced physiotherapist.
- Emotions management, if there is no emotional regulation despite the individual's will, it is necessary to seek the help of a psychologist.
The fact that there are coping strategies indicates that there is an exercise of will, a cognitive effort that can be translated into behavioral modifications to better adapt to its new reality, indicates that you are fighting with the best weapons available.
"Behind the smile of a person suffering from chronic pain, a battle is implied to the invasive tyrant".

Breastfeeding and chronic pain
A large part of patients suffering from chronic pain are women, many of them are or intend to be mothers. Breastfeeding the baby is great benefits to the health of mother and son, chronic pain is another reason to promote the benefits of breastfeeding and being a "good chest", as Melanie Klein said.
The researchers observed that After a caesarean section, the mothers who tied their newborn, for a period of at least two months, showed being less prone to pain, Regarding those who did not breastfeed their baby. Feeding the kid in this way, strengthens the maternal bond, the immune system of both, especially the neonate, while "emotional skin is tone", making it more resistant to emotional fragility.
Deadaptive coping strategies
They are the ones that have to do with avoidative behaviors, through research, this type of passive strategies have been correlated negatively, since they affect the chronicity and intensification of pain, consuming the well -being of the person gradually. Chronic pain, due to its characterology, it generally also implies a great emotional discomfort for those who suffer from it.
The type of passive coping with pain has been associated with the increase in: feelings of impotence, cognitive evaluation with bias in the negative, anxiety and depression, among others. These strategies include Desiderative thought, where the person lives in the illusion that everything will be better, waiting without making the necessary adjustments for it, Just by believing and wishing it so, it can affect important decision making, its optimism, is based on a belief without foundation in reality.
The scientists also realized that: "Ignore pain”, It represents avoidance, people suffering from Álgic syndrome must be attended by specialized health professionals for it, represents a right and WHO (World Health Organization) recognizes it as a condition that should be treated as such ( 2017), When there is this type of beliefs, they can lead to the patient not to follow medical indications, thus aggravating their condition.
On the other hand, it is a good strategy to try to focus attention on something different from pain, when medical indications were already followed, the possible was done to relieve it and endures. Other passive coping strategies are affective and physical isolation, which contributes to the exacerbation of mood disorders, irritability, aggressiveness (Fishbain, 2000), feelings of guilt and shame, which must be transcended, to potentiate your skills, Well, a body that keeps blame seeks often seeks to punish. If you cannot remove pain on yourself, you can lighten emotional suffering, the latter can be optional, the first must be understood as a condition that is often not in your hands to change. Hippocrates is attributed to the phrase:
"Divinum opus sedare painm est" ... "Calm pain is a divine task."
Health professionals specialized in pain identify with this phrase, as in the mythology Prometheus tried to take fire for the good of humanity, recognizing the titanic of their work, so they, hand in hand with neurosciences They study the ways in which the person can relieve their pain or suffer less and offer a better quality of life to their patients.
Conclusion
"Who has a reason to live will find a how"Friedrich Nietzsche.
The adaptation of the individual to their living conditions different from the above, is necessary to seek more well -being, although it is true that many times the pain is inevitable, The patient can learn coping techniques to influence psychological variables that directly affect their health and that at the same time they can make pain intensify or reduce. You don't have to free this battle, Psychological accompaniment and treatment are optimal to generate good effects on pain perception.
Links
- DOI: 10.1038/SREP19615
- DOI: 10.5665/Sleep.5158
- http: // www.Redalyc.org/html/970/97017363002/
- https: // www.Nature.com/articles/s41467-018-04309-2
- https: // neurosciencenews.com/front-lobe-chronic-pain-9148/
- https: // neurosciencenews.com/BREASTFEEDING-PAIN-C-SECTION-6834/
- https: // mh.BMJ.com/content/43/3/155
- https: // linkinghub.Elsevier.com/retrieve/pii/s1526590004006650

